Every breath you take depends on a hidden cellular “switch” now rewriting what we know about healing—and failing—lungs, with consequences that could transform medicine.
Story Snapshot
- Scientists at Mayo Clinic uncovered a molecular “switch” in lung cells dictating repair or immune defense.
- This discovery upends decades of assumptions about how our lungs recover from disease and injury.
- The finding unlocks new paths for regenerative therapies in chronic lung conditions like COPD and fibrosis.
- Translating this mechanism into treatment could mean the difference between organ failure and recovery.
Cellular Fate in the Lungs: The Unexpected Division of Labor
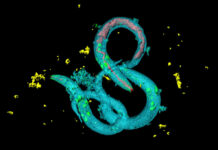
Researchers at Mayo Clinic announced the discovery of a molecular circuit in alveolar type 2 (AT2) lung cells that acts as a decision-making “switch,” forcing each cell to specialize in either repairing tissue or mounting immune defense—but never both at once. This finding, published in Nature Communications, challenged the long-held belief that AT2 cells could simultaneously juggle healing and protection. For decades, textbooks described these cells as multi-taskers, but new single-cell sequencing and imaging revealed a binary fate hardwired deep within our lung tissue.
Scientists concerned after 'surprising' discovery deep in the lungs of every living person: 'We did not expect to find [this]' – The Cool Down https://t.co/z4y0LeQRxb
— Rich Newbold (@drnewbold) November 15, 2025
Lead researcher Dr. Douglas Brownfield, Ph.D., said, “We were surprised to find that these specialized cells cannot do both jobs at once… That division of labor is essential.” The surprise wasn’t just academic. In chronic lung diseases, the failure of these cells to regenerate damaged tissue is a key reason why lungs deteriorate. Now, with the “switch” identified, scientists see an opportunity to intervene before repair breaks down entirely.
Unlocking Regeneration: The PRC2, C/EBPα, and DLK1 Circuit
The molecular “switch” involves a trio of regulators—PRC2, C/EBPα, and DLK1—dictating whether AT2 cells focus on regeneration or defense. C/EBPα, in particular, acts as a clamp, preventing AT2 cells from reverting to a stem-cell-like state when the body shifts to immune defense mode. This revelation explains why, in diseases like pulmonary fibrosis and severe viral infections, the lungs often lose their ability to heal: the switch gets stuck, locking cells into a defensive posture when repair is desperately needed.
From Discovery to Therapy: The Road Ahead
The implications reach beyond the lab. Chronic lung diseases like COPD and fibrosis affect millions, with limited options once damage accumulates. The Mayo Clinic’s discovery suggests that early detection of an imbalanced “switch” could serve as a biomarker, warning of impending disease before symptoms appear. This fits squarely within the Clinic’s Precure and Genesis initiatives, which focus on early detection and regenerative medicine for organ failure. Other research centers, like UCLA, are now using advanced lung organoids—miniature lungs grown in the lab—to probe how this molecular circuit operates in different disease states.
Changing the Future of Lung Medicine
Experts across the field agree that this discovery fundamentally changes the conversation about how and when lungs can heal. Some caution that translating these findings into clinical therapies will take time and rigorous trials. Yet, the consensus is clear: understanding the division of labor in AT2 cells transforms our ability to diagnose, prevent, and eventually cure chronic lung diseases.
The economic and social stakes are enormous. Regenerative therapies could slash healthcare costs, reduce hospitalizations, and restore quality of life for millions. For patients and families facing relentless lung decline, this molecular “switch” might soon become the on-off lever for hope.
Sources:
Science Daily: Mayo Clinic researchers discover molecular “switch” in lung cells
UCLA Stem Cell: Scientists create first mini-lungs with blood vessels
Mayo Clinic News Network: New discovery may unlock regenerative therapies for lung disease
University of California News: Scientists create first mini-lungs built with blood vessels